Is Healthy Poop Soft or Hard? The Ideal Stool Explained
We’ve all been there – sitting on the toilet, struggling to pass a rock-hard bowel movement. You strain and grunt, hoping this stubborn poop will somehow make its way out. The whole experience leaves you red-faced and irritated.
On the flip side, there’s the loose, watery stool that dumps out in an urgent, explosive mess. You barely make it to the bathroom in time before your insides turn to liquid. Talk about a crappy situation!
So what does healthy poop look like? The ideal stool is soft and easy to pass but still maintains a solid, sausage-like shape. Think of a smooth snake slithering its way out or soft-serve ice cream flowing through the bowl. This means your poop has the right amount of water and nutrients in it when you pass it.
According to the Bristol Stool Chart, the healthiest poops are types 3 and 4. Type 3 is a log shape with cracks in the surface. Type 4 resembles a smooth snake. Poops that are too hard or too liquidy can signal problems like constipation or diarrhea.
The good news is you can improve your poop quality with some simple diet and lifestyle tweaks. In this post, we’ll explore what your poop is telling you and how to get your bowel movements back on track. Let’s get to the bottom of healthy pooping!
The Goldilocks Poop: Not Too Hard, Not Too Soft
Healthy poop should be soft and easy to pass, but still maintain a solid, sausage-like shape. Think of a smooth snake slithering out or soft-serve ice cream flowing through – that’s the poop sweet spot.
Specifically, your stool should:
- Have a solid consistency: It shouldn’t be loose or liquidy. A healthy poop holds its shape when it hits the bowl.
- Be about 1-2 inches wide: The ideal width is similar to a banana or your index finger.
- Range from 4-8 inches long: Length can vary from a short snake coil to an extended log.
- Be easy to pass: You shouldn’t have to strain, grunt, or push excessively.
- Feel “complete”: You should feel empty when you’re done and not have the urge to poop again soon after.
If your poop cracks apart in the bowl or comes out in small pebbles or pellets, that’s also considered normal and healthy.
The right poop consistency shows your stool has an optimal amount of water and nutrients as it passes through you. Think of it like moist, compacted soil that holds its structure.
Decoding the Bristol Stool Chart
Gastroenterologists often refer to the Bristol Stool Chart, which categorizes poop into 7 types based on shape and texture:
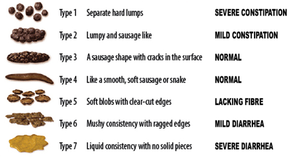
Types 3 and 4 are considered ideal on this chart.
- Type 3 is a sausage-like log with cracks in the surface. Also described as “smooth snakes”.
- Type 4 is a smooth, soft poop shaped like a snake.
These types signify a healthy transit time and full absorption of nutrients from your food. Your digestive system is working properly!
Conversely, Types 1 and 2 indicate constipation, while Types 5-7 signal diarrhea or urgency. We’ll explore the causes of unhealthy poop later.
What Makes the Perfect Poop?
A few key conditions in your body create that coveted soft, solid poop:
- Adequate fiber intake: Fiber adds bulk and moisture to stool, while stimulating movement through the colon. Shoot for 25-35 grams daily through foods like beans, oats, berries and veggies.
- Proper hydration: Water keeps your poop soft. Men should drink 15 cups of fluids daily, while women need 11 cups. Focus on water over diuretic drinks like coffee.
- Regular physical activity: Moderate exercise helps food waste move through your system via muscular contractions. Aim for 150 minutes per week.
- Healthy gut flora: The trillions of bacteria in your intestines aid digestion and stool formation. Eat probiotic foods like yogurt, kefir and sauerkraut to maintain balance.
- No underlying conditions: Certain medical issues like IBS, infections, hemorrhoids, etc can affect poop consistency. See a doctor if problems persist.
Think of your colon like a well-oiled machine – with the right inputs like fiber and fluids, it will produce a consistently smooth output.
Hard, Pellet-Like Stool (Types 1 and 2)
Stools at the opposite end of the spectrum, classified as Types 1 and 2, are hard, dry and tough to pass. You may feel like you’re pooping out rocks or tiny rabbit pellets.
This often signals constipation – where stool moves too slowly through the digestive tract, resulting in excess water absorption. Constipation is extremely common, affecting up to 20% of Americans.
What causes it?
- Not enough fiber: Without adequate roughage from foods like vegetables, fruit and whole grains, stool remains dense and compacted.
- Dehydration: When lacking fluids, the colon pulls water from poop, making it stiff.
- Sedentary lifestyle: Without regular activity, contractions in the colon weaken, slowing motility.
- Certain medications: Antacids with calcium and iron, anti-depressants, blood pressure drugs and others may induce constipation.
- Chronic disease: Diabetes, multiple sclerosis, lupus and thyroid disorders can impair digestive function.
- Bowel obstruction: Slowed motility may result from a blockage like a tumor or impacted feces.
- Irritable bowel syndrome (IBS): Changes in the colon’s contractions cause infrequent, strained BMs.
- Resisting the urge to poop: This causes stool to harden and dry out in the rectum.
To alleviate constipation, focus on getting more exercise, fluids, fiber and probiotic foods. Take any problematic medications with caution. If the problem persists, see your doctor to rule out underlying conditions.
In severe cases, laxatives or stool softeners may provide short-term relief, but don’t rely on these long-term without medical supervision.
Loose, Watery Stool (Types 5-7)
On the flip side of constipation, stool can also be too loose or liquid-y, like Types 5-7 on the chart.
This usually signals diarrhea – where food transits the colon rapidly without enough water being absorbed back into the body. The result is an urgent, explosive bowel movement.
Diarrhea strikes most people occasionally and can result from:
- Food poisoning: Bacteria like e. Coli or Salmonella from spoiled food can infect the digestive tract.
- Viruses: The stomach flu, norovirus and rotavirus often cause bouts of diarrhea.
- Parasites: Giardia from contaminated water and other parasites lead to intestinal infection.
- Food intolerance: Lactose, fructose or sugar alcohols may not be properly digested, drawing fluid into the colon.
- Chronic disease: Celiac, IBD and IBS involve intestinal inflammation or irritation.
- Reaction to medicines: Antibiotics, heartburn drugs, and chemotherapy commonly induce diarrhea.
- Stress and anxiety: The gut is highly sensitive to emotions via the gut-brain connection.
To curb diarrhea, drink plenty of fluids, rest, and stick to a bland diet like the BRAT method until symptoms subside: Bananas, Rice, Applesauce, Toast. Over-the-counter anti-diarrheals can provide relief in moderation. Call your doctor if diarrhea lasts over 3 days or is accompanied by fever, blood or dehydration.
When to Worry about Poop Consistency
While occasional bouts of constipation or diarrhea are normal, ongoing poop problems can signal underlying issues. See your doctor if you experience:
- Changes in poop that last over 2 weeks
- Blood in stool
- Intense cramping or pain
- Unexplained weight loss
- Fever or dehydration
Keep a journal tracking your poop frequency, consistency, color and comfort level to help pinpoint patterns.
Certain high-risk groups like young kids, elderly and immunocompromised individuals should take special care to stay hydrated and notify a doctor about major poop changes.
Tips for Assessing Your Poop
Paying attention to your poop provides vital clues about your health. Some tips:
- Note the frequency: Pooping 3x a day to 3x a week is generally normal. Outside this range may indicate problems.
- Check your comfort: Healthy poop requires little straining. Pain can mean issues like hemorrhoids or fissures.
- Observe shape and texture: Use the Bristol Stool Chart types. Consistency can vary day-to-day but look for prolonged changes.
- Watch for color: Brown is normal, but black, yellow, or red hues may mean something is wrong.
- Consider supplements: Probiotics, magnesium, and vitamin C are popular for improving regularity.
- See your doctor: If your poop looks consistently unusual or you have persistent discomfort, seek medical advice.
Pooping While Traveling
Of all the bodily functions you don’t want to have trouble with away from home, pooping tops the list! Unfortunately, travel often disrupts normal bathroom habits.
Motion sickness, jet lag, schedule changes and unfamiliar food can influence your poop. Plus the stress of transit and new locations impacts your digestion.
Here are some tips for maintaining healthy poop while traveling:
- Hydrate, hydrate, hydrate: Drink plenty of fluids, starting a few days before departure. Water and diluted juices are ideal.
- Eat probiotic-rich foods: Stock up on yogurt, kefir, sauerkraut and kombucha which can ease stomach upset.
- Bring key supplements: Travel with fiber supplements and probiotics to maintain your regimen.
- Avoid problem foods: Greasy or spicy foods and sugar alcohols found in gum and diet drinks can cause diarrhea.
- Don’t resist the urge: Holding it on planes or buses can exacerbate constipation. Use the bathroom when needed.
- Exercise: Even light walking or stretches at rest stops keeps things moving through your system.
- Beware new medications: Talk to your doctor before taking anti-diarrheals or laxatives when away from home.
If poop problems arise, drink fluids with electrolytes, rest, and stick to mild, bland foods. You can also find probiotics and dietary supplements abroad. Seek medical attention for severe issues.
Pooping After Surgery
Undergoing surgery and anesthesia takes a major toll on your digestive function. Bowel regimens are often a central focus of post-op recovery.
Being immobile plus strong pain meds reduce colon activity. This leads to issues like:
- Constipation: Opioids cause the intestines to soak up more fluid, hardening stool.
- Diarrhea: Some meds loosen stools while digestive muscles heal.
- Straining: Pushing too hard can damage surgical incisions and stitches.
Doctors usually recommend:
- Advance warning: Notify your surgeon if you have a history of constipation or diarrhea before surgery.
- Stop eating: Halt intake of solid foods 6-12 hours pre-op to empty bowels.
- Start laxatives: You’ll need to clean out your system before going under anesthesia.
- Continue stool softeners: Stay ahead of post-op constipation with docusate and other softeners.
- Eat high fiber: Gradually resume a high fiber diet as you can tolerate solid foods.
- Stay active: Light walking encourages motility when approved by your doctor.
- Consider probiotic supplements: These can ease side effects of antibiotics often given before or after surgery.
- Avoid straining: Don’t push extremely hard if constipated. Call your surgeon if pooping is painful.
With diligence, supplements and patience, most patients can get back to regular, healthy pooping after recovering from surgery. But don’t hesitate to ask for help managing bowel issues from your medical team.
Pooping During Pregnancy
Pregnancy brings enough bodily changes without turning your poop weird too. But hormone surges definitely affect digestion. Plus, that growing baby compresses your colon.
Some common poop problems during pregnancy include:
- Constipation: Progesterone relaxes muscles, slowing motility. Iron supplements prescribed for anemia also bind you up.
- Hemorrhoids: Pressure from the uterus and pushing during labor can inflate veins in the anus.
- Diarrhea: Hormone changes can stimulate loose stools at times. Some women alternate between constipation and diarrhea.
- Discomfort: Sitting and wiping becomes more difficult. You may actually miss those normal pre-pregnancy poops!
To keep your poop on track while expecting:
- Drink more fluids: Shoot for 10 cups daily, favoring water and juice over diuretics like coffee.
- Load up on fiber: Bran cereal, fruit, veggies and whole grains help move things along.
- Exercise: Walking, swimming, yoga and kegels promote healthy circulation.
- Try probiotics: These support your changing microbial balance and immunity.
- Discuss medications: Get approval before using stool softeners, laxatives or anti-diarrheals.
- Consider supplements: Magnesium, vitamin C and omega-3s may improve regularity.
- Go when needed: Answer any bowel urges promptly to avoid straining later.
- Relieve hemorrhoids: Soak in warm baths, use wipes, and try topical creams or cold compresses.
If poop problems persist, tell your OB-GYN. They can check for impactions or obstetrical complications. Stay vigilant about hydration and nutrition for your own health plus proper fetal development.
Pooping After Childbirth
While delivering your precious baby is joyous, pooping after childbirth often feels anything but beautiful. Between raging hormones, pain meds, stitches and sheer exhaustion, that first postpartum poop can be downright frightening.
However, clearing out your system promotes healing and recovery. Move those bowels gently with:
- Water: Hydration softens things up and prevents or relaxes constipation.
- High fiber foods: Introduce grains, raw veggies, fruits, nuts and seeds gradually.
- Stool softeners: Discuss docusate, glycerin suppositories or other options with your provider.
- Laxative teas: Many moms find teas with senna or flaxseed effective.
- Probiotics: Replenish healthy gut flora shaken up by antibiotics. Yogurt and kefir are great options.
- Exercise: Light walking encourages motility when approved by your doctor.
- Take your time: Allow gravity to help and don’t force it. Pooping may not happen for 3-5 days.
- Support your perineum: Place a pad, witch hazel pad or frozen maxi pad over stitches to ease straining.
- Consider a squatty potty: Elevating your feet simulates a squat position for easier elimination.
Call your OB-GYN if you haven’t pooped after 5 days or experience painful bowel movements, bleeding or dizziness. Take it slow but stay proactive about pooping after labor.
Maintaining Healthy Poop Across Your Life
Hopefully this crash course gives you confidence to assess your poop consistency and take steps to achieve the ideal stool. Keeping your colon moving efficiently provides huge benefits to your comfort, health and quality of life at every age.
While poop patterns fluctuate day-to-day, pay attention for prolonged changes in stool consistency plus any pain or straining during bowel movements. Don’t ignore the clues your poop provides!
Stay proactive by drinking plenty of fluids, eating 25-35 grams of fiber daily, exercising moderately and considering probiotic supplements. And never hesitate to discuss poop problems with your doctor – as embarrassing as it may seem, they really have heard it all!
Our poop mirrors the state of our gut health and overall wellbeing. With proper care and awareness, you can keep your bowel movements moving smoothly for years to come.
